High Cholesterol
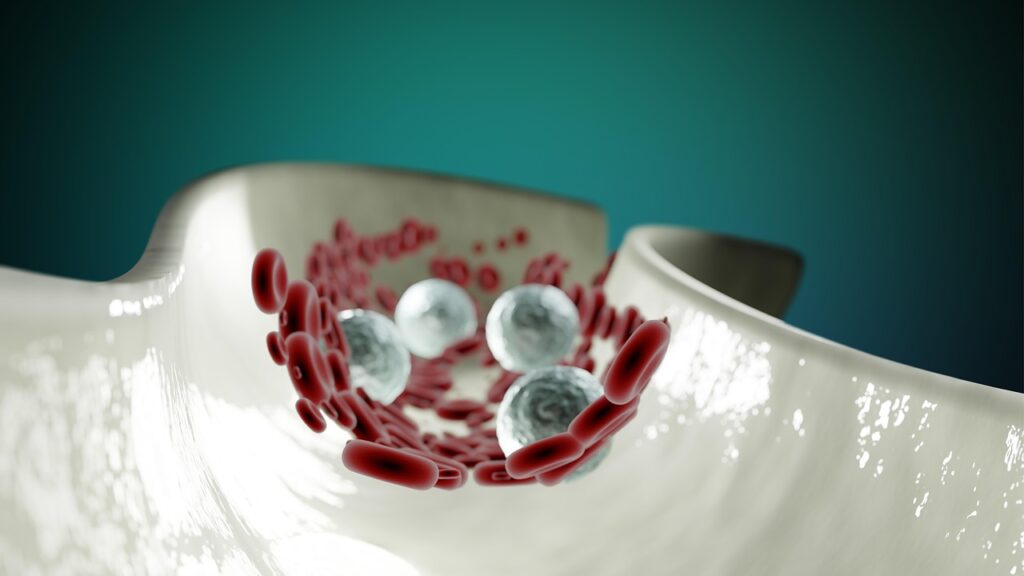
High cholesterol is a condition where excess cholesterol builds up in the bloodstream, increasing the risk of heart disease and stroke. Often symptomless, it can go unnoticed until it causes serious complications—earning it the reputation of a “silent threat.”
Symptoms and Causes
High cholesterol typically has no symptoms, which is why regular screenings are crucial. It often results from a combination of genetics and lifestyle choices like a diet high in saturated fats, lack of physical activity, smoking, or excess alcohol consumption. Elevated LDL (“bad”) cholesterol contributes to arterial plaque, while low HDL (“good”) cholesterol can also raise cardiovascular risk.
Prevalence and Prognosis
Nearly 40% of U.S. adults have high cholesterol, and many are unaware of it. The good news: it’s manageable. Through lifestyle changes, medication, and regular monitoring, the risks associated with high cholesterol can be significantly reduced.
Management and Treatment
- Diet: Eating more fiber, whole grains, lean proteins, and healthy fats while reducing saturated and trans fats can help manage cholesterol levels.
- Exercise: Regular physical activity can increase HDL cholesterol and lower LDL cholesterol and triglycerides.
- Medications: Statins are most common, but others like ezetimibe, PCSK9 inhibitors, or bile acid sequestrants may be prescribed.
- Lifestyle Changes: Quitting smoking, limiting alcohol, managing stress, and maintaining a healthy weight are key to long-term control.
Living with High Cholesterol
Successfully managing cholesterol means being proactive: regular checkups, adherence to prescribed plans, and maintaining healthy habits. Support from loved ones and healthcare providers can make this ongoing process more manageable and sustainable.
Common Concerns for Individuals Managing High Cholesterol
Risk of Serious Complications
If left uncontrolled, high cholesterol can lead to coronary artery disease, heart attacks, strokes, and peripheral artery disease. Managing cholesterol levels is vital for cardiovascular health.
Monitoring and Testing
Regular blood tests are necessary to track cholesterol levels. Many people find interpreting their results—especially newer or more advanced markers—challenging.
Medication Side Effects
Side effects like muscle aches, digestive issues, or liver enzyme elevations can be concerns with statins and other cholesterol-lowering medications, leading to questions about long-term use.
Nutrition and Food Choices
Switching to a cholesterol-friendly diet can feel overwhelming. Learning to read food labels and avoid hidden fats or sugars is a frequent concern.
Exercise and Physical Activity
Starting or maintaining an exercise routine can be tough, especially with existing health issues. Tailoring physical activity to your ability and preferences is key.
Stress and Emotional Well-being
Stress can affect eating, sleep, and exercise habits. Finding effective ways to manage it—like mindfulness, therapy, or creative outlets—supports overall heart health.
Managing Other Conditions
Cholesterol issues often coexist with conditions like diabetes, hypertension, or obesity. Coordinated care is essential for managing multiple risk factors.
Cost and Access to Care
The financial burden of medications, tests, and doctor visits can be significant. Access to affordable and consistent care is a common concern.
Awareness and Education
Understanding terms like LDL, HDL, triglycerides—and now Lp(a)—isn’t always straightforward. Staying informed empowers better choices and discussions with your healthcare provider.
Understanding Lp(a): The Hidden Cholesterol Risk
Lipoprotein(a), or Lp(a), is a type of cholesterol particle that carries a particularly sticky form of LDL. Elevated Lp(a) levels are largely genetic and are not typically affected by diet, exercise, or most standard cholesterol medications.
Why It Matters
High levels of Lp(a) are linked to a significantly higher risk of heart attack, stroke, aortic valve disease, and blood clots—even in people with normal LDL levels. It’s an independent risk factor and often goes untested in routine cholesterol panels.
How to Test
A simple blood test can measure Lp(a) levels, but it’s not included in standard cholesterol screening. If you have a personal or family history of early heart disease or stroke, talk to your doctor about getting tested.
Managing High Lp(a)
While lifestyle changes still matter, elevated Lp(a) often requires more targeted interventions:
- Niacin has shown limited success in lowering Lp(a), but its use is now less common due to side effects.
- PCSK9 inhibitors may reduce Lp(a) in addition to LDL.
- New therapies specifically targeting Lp(a) are in development and showing promise in clinical trials.
Understanding and monitoring Lp(a) is an important step for individuals at high cardiovascular risk—especially when traditional risk factors don’t tell the full story.
Featured in High Cholesterol
- Sticky Stuff: What’s Lp(a) and How to Keep It from Cluttering Your Arteries
 If you’ve never heard of Lp(a), don’t worry—you’re not alone. Most people haven’t, and it’s not because it’s not important.…
If you’ve never heard of Lp(a), don’t worry—you’re not alone. Most people haven’t, and it’s not because it’s not important.… - Your ‘Normal’ Blood Pressure Reading Could Be Dangerously Wrong
 You go for your annual checkup, and the doctor says, “Your blood pressure looks normal—120/80.” You breathe a sigh of…
You go for your annual checkup, and the doctor says, “Your blood pressure looks normal—120/80.” You breathe a sigh of… - Eat Your Way to Happier Hips & Knees
 If you’re an arthritis warrior, you know that sometimes your joints feel like they’ve auditioned for a role as a…
If you’re an arthritis warrior, you know that sometimes your joints feel like they’ve auditioned for a role as a… - Metabolism Makeover: The Shocking Secret to Burning Fat Without Dieting
 Most weight loss articles promise quick fixes and miracle solutions. This isn’t one of them. Instead, we’re going to explore…
Most weight loss articles promise quick fixes and miracle solutions. This isn’t one of them. Instead, we’re going to explore… - Genetic Lottery: How Your DNA Determines Your Health Destiny (And What You Can Do About It)
 Ever wonder why some people seem to eat whatever they want and never gain a pound, while others just look…
Ever wonder why some people seem to eat whatever they want and never gain a pound, while others just look… - Processed Foods Exposed: The Billion-Dollar Industry Gambling with Your Longevity
 If you’ve ever grabbed a bag of chips, scarfed down a frozen dinner, or sipped on a sugary soda, you’re…
If you’ve ever grabbed a bag of chips, scarfed down a frozen dinner, or sipped on a sugary soda, you’re… - Superfoods vs Supplements: What Big Nutrition Doesn’t Want You to Know
 If you’ve ever found yourself staring at a bottle of vitamins and wondering if you should just eat an avocado…
If you’ve ever found yourself staring at a bottle of vitamins and wondering if you should just eat an avocado… - Berries to the Rescue for Joint Relief
 When it comes to arthritis or other inflammatory conditions, berries might just become your new best friends. These tiny, colorful…
When it comes to arthritis or other inflammatory conditions, berries might just become your new best friends. These tiny, colorful… - Brain Games or Snake Oil? What Actually Helps Your Memory
 With a sea of apps, supplements, and puzzles claiming to supercharge your brain, it’s hard to separate fact from fiction.…
With a sea of apps, supplements, and puzzles claiming to supercharge your brain, it’s hard to separate fact from fiction.…

